Washington University School of Medicine researchers have cured a type of diabetes in mice using the CRISPR gene editing tool.
Diabetes is caused when the islet beta cells of the pancreas stop producing insulin (Type 2), which is essential for controlling blood sugar levels, or when genetic mutations result in the inability of the cells to produce insulin (type 1). It has been estimated that around 415 million people worldwide have diabetes, or 1 in 11 of the world’s population. The type of diabetes cured by the researchers is a rare form of type 1 diabetes called Wolfram syndrome.
The study was conducted to correct Wolfram syndrome because this form of diabetes is caused by a mutation in a single gene, which is more straightforward to correct using CRISPR than mutations in multiple genes. “This is the first time CRISPR has been used to fix a patient’s diabetes-causing genetic defect and successfully reverse diabetes,” said co-senior investigator, Jeffrey R. Millman, PhD, assistant professor of medicine and biomedical engineering at Washington University. “We see this as a stepping stone toward applying gene therapy to a broader population of patients with diabetes.”
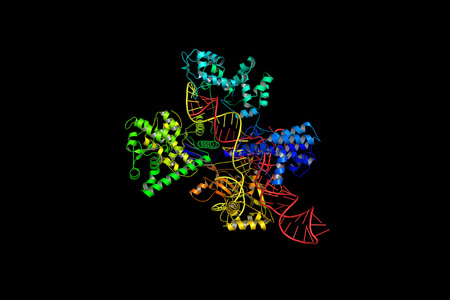
In their study, the researchers harvested fibroblast skin cells from a patient with Wolfram syndrome, converted the cells to induced pluripotent stem cells (IPSCs) in the lab, then corrected the genetic defect that caused Wolfram syndrome using CRISPR-Cas9. In their study, the beta cells grown in the lab and used in the treatment were indistinguishable from the beta cells of healthy individuals who do not have diabetes.
The genetically engineered cells were injected into a mouse model with Wolfram syndrome. After treatment, mice were able to start producing near normal levels of insulin and continued to do so for 6 months following treatment until the end of the study. If the treatment were to be provided to humans, it would mean that insulin injections would no longer be required by patients. There is no guarantee that the treatment would work in humans, but the researchers are optimistic that their technique could be used in novel treatments for type 1 and potentially other forms of diabetes. Since cells can be harvested from a patient, converted into IPSCs in the lab, and then reintroduced back into the same patient, problems of rejection of the cells would be overcome.
One of the problems that can occur when creating beta cells from IPSCs is that the differentiation process is dificult to precisely control and in addition to generating beta cells, other cell types are also generated. While introducing these other cell types – liver cells for example – will not cause any harm, it would reduce the effectiveness of the treatment. The researchers’ 6-stage differentiation strategy solved this problem and ensured that sufficient numbers of beta cells were created from IPSCs to allow diabetes to be cured.
You can read more about the study in the paper – Gene-edited human stem cell-derived ß cells from a patient with monogenic diabetes reverse pre-existing diabetes in mice– which was recently published in the journal Science Translational Medicine. DOI: 10.1126/scitranslmed.aax9106