One of the problems of using an adeno-associated virus (AAV) to deliver gene editing tools into cells, is the immune system may recognize the virus as foreign, develop antibodies against the virus, and eradicate it before any editing has taken place. This immune response has caused many clinical trials of gene therapies to fail. Once immunity to the virus has been developed, if the virus is re-introduced, the immune system would simply eradicate the virus again.
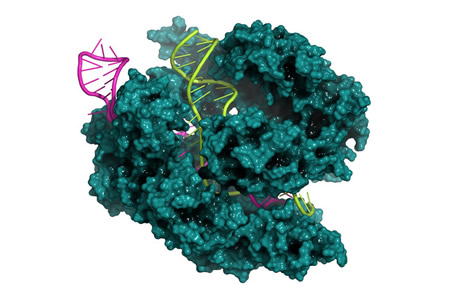
CRISPR-Cas9 is a gene editing tool that can be used to insert functional genes and correct mutations, but the system can also be modified (by truncating the guide RNA) to allow the Cas9 protein to be used for transcriptional modulation of genes. Using CRISPR to provide transcriptional control over the genes responsible for immunity could potentially help to improve the efficacy of gene therapies, by reducing the potential for the immune system to attack the AAVs used to deliver the tools used to perform the necessary edits to the DNA.
A team of researchers have used this approach and have shown it is possible to simultaneously use CRISPR to target a gene involved in immune signaling, while also using CRISPR for gene therapy. The researchers developed a CRISPR-based transcriptional repressor system that gave them transcriptional control and also allowed gene editing to be performed on demand.
The researchers targeted the myeloid differentiation primary response 88 (MyD88) gene, which plays a critical role in innate and adaptive immune signaling pathways. The gene is also important for forming adaptive immunity to AAVs and in the response to septicaemia.
Two transcriptional repressors were fused – heterochromatin protein 1 (HP1a) and Krüppel-associated box (KRAB) – to the MS2 coat that is recruited by a gRNA aptamer binding to a nuclease-competent CRISPR complex containing truncated gRNAs. The enhanced CRISPR-based transcriptional repressor was then used to reprogram immune homeostasis in vivo.
“We demonstrate transcriptional repression of the Myeloid differentiation primary response 88 (Myd88) gene in vitro and in vivo. We demonstrate that this strategy can efficiently downregulate Myd88 expression in lung, blood and bone marrow of Cas9 transgenic mice that receive systemic injection of adeno-associated virus (AAV)2/1-carrying truncated gRNAs targeting Myd88 and the MS2-HP1a-KRAB cassette,” explained the researchers.
Myd88 levels in the blood were reduced by 84%, there was a 75% reduction in the lungs, and a 63% reduction in the bone marrow. “This downregulation is accompanied by changes in downstream signalling elements such as TNF-α and ICAM-1. Myd88 repression leads to a decrease in immunoglobulin G (IgG) production against AAV2/1 and AAV2/9 and this strategy modulates the IgG response against AAV cargos.”
The researchers then used this approach to pretreat mice before delivering AAV9-based gene therapies at 7 and 14 days. Mice that were pretreated with the CRISPR-based transcriptional repressor has lower levels of immunoglobulin against the pretreatment (AAV1) and gene therapy (AAV9) viruses.
This suggests that using the repressor prophylactically can improve the efficacy of gene therapy. The researchers also demonstrated the CRISPR-based transcriptional repressor can be used to prevent sepsis by stopping the upregulation of inflammatory markers, and could potentially be used to prevent inflammatory responses and the resultant tissue damage involved in other inflammatory conditions, including COVID-19.
You can read more about the research in the paper – Synthetic immunomodulation with a CRISPR super-repressor in vivo – which was recently published in the journal Nature Cell Biology. DOI: 10.1038/s41556-020-0563-3